The Isle of Man’s battle against coronavirus took a giant leap forward last week when the on-island testing lab opened for business.
It is now possible to complete up to 200 tests every day at Noble’s Hospital. Testing will be an essential part of the gradual steps towards a less restricted future, writes Dave Kneale.
For Stephen Doyle (pictured below), pathology manager at Noble’s Hospital, it has been an eventful few weeks: ’If somebody had said to me two months ago that we’d have this testing ability on the Isle of Man, even in the next five or 10 years, I wouldn’t have believed them.’
With collaboration between the government, private enterprise and well-wishing members of the public, it took the entire island community pulling together to make it happen. And yet the journey to a world-class testing operation began with a chance discovery.
In early March - weeks before the first case was confirmed in the island - Mr Doyle was faced with a problem: Public Health England could only promise a limited number of Covid-19 tests a day, which wouldn’t be enough to contain any outbreak.
Dr Rachel Glover, a molecular biologist and chief scientific officer for Onchan-based Taxa Genomics, could see the issue. Presuming that the gold standard of coronavirus testing - a real-time PCR machine - was beyond the island’s capacity, she concluded that her equipment would be the next best thing.
’I thought that we could come up with some kind of interim testing solution,’ Dr Glover said.
’At the time I didn’t think we had a real-time PCR testing machine on the island.’
Nor did anyone else until March 17. That was when senior microbiologist Chris Helm checked out some equipment in the government Analyst’s Laboratory.
He left the lab with the holy grail packed up in the boot of his car. The machine had originally been purchased for environmental testing, years before the coronavirus pandemic turned it into one of the world’s most sought-after medical devices.
’It’s the exact model that Public Health England are using for their COVID testing’, Dr Glover said.
’It’s like finding a brand new car, that’s had a dust sheet over it in a garage for the last 10 years.’
It was an incredible stroke of luck. But it wasn’t the only one in this story.
Having the equipment was one thing, actually using it to develop a solid testing process was another.
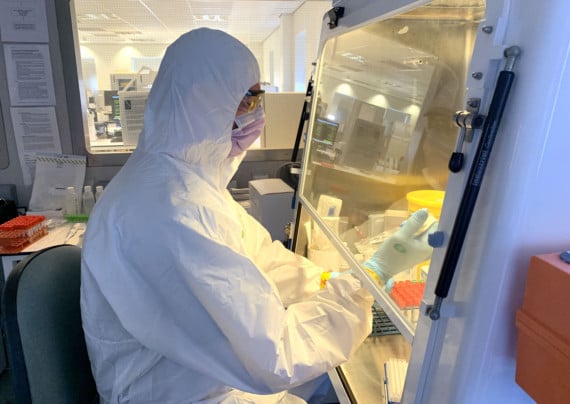
Step forward Dr Glover (pictured right): ’I worked for DEFRA in the UK as a scientist for many years, designing, deploying and validating exactly this type of testing for plant health and food security,’ she explained.
She was immediately seconded to the pathology lab at Noble’s, where weeks of work began with head of microbiology Rebecca Shields and a team of biomedical scientists.
On-island testing was more than just a partnership between government and the private sector. When an essential component got stuck at East Midlands Airport on March 28, the community stepped in to deliver the goods. Thanks to a nudge from Douglas North MHK Ralph Peake, Manx resident John Whittaker lent his private helicopter while the Government Secretary signed a last-minute exemption to the border closure.
The part was in the lab by the afternoon. ’I don’t think it could happen anywhere else,’ Mr Doyle said.
’It’s a great example of what can happen in the Isle of Man when everyone decides to get things done.’
It became more urgent for the Isle of Man to chart its own course as the crisis deepened in the UK.
For weeks, the lab in Manchester had been returning results by the hundred.
But as the UK finally committed to mass testing, Mr Doyle said, the island was riding its luck: ’We could have got to the stage where they were rationing the number of tests they were doing for us.’
The final decision to switch to local testing was made on April 17, exactly a month after the crucial piece of equipment had been found. To confirm the results were accurate, everyone tested at the Grandstand over the previous 10 days had been ’double-swabbed’ - one sample was sent to the lab in Manchester and the other was processed at Noble’s Hospital.
’The double swab tests fully validated our method, along with internal quality control measures’, Mr Doyle said.
Nevertheless the first week’s results saw a huge drop in confirmed cases, prompting some nervous questions on social media - was there a problem with the local testing?
Mr Doyle said that the cluster of cases at Abbotswood nursing home, which arrived just before the switchover, had obscured the bigger picture - that the infection rate in the community has fallen dramatically. ’We keep in very close contact with the other UK overseas territories and Crown Dependencies,’ he explained.
’All the island nations are seeing the same pattern, where the numbers are dropping off a few weeks after the borders are closed.’
Between the border closure, lockdown and the efforts of the Manx community, there are encouraging signs that the first wave of coronavirus has been suppressed. But testing and tracing are the building blocks of everything that comes afterwards.
Restrictions can only be eased with constant monitoring through community testing - the quick turnaround time at Noble’s will be crucial in detecting and containing the virus.
The Examiner can reveal that the island’s testing capacity could be doubled to up to 400 results per day, using the existing equipment, as the process is refined over the next few weeks.
Meanwhile, in another minor miracle, Taxa Genomics have acquired a second testing machine. Should there be a ’second wave’ of infection it could boost the island’s testing capacity even further.
’If there was a surge in cases, we’re in a good place to be able increase, again, our testing capacity’, Mr Doyle said.